Does it seem like you’ve heard diabetes being mentioned more than usual? This is because diabetes is quickly becoming a priority healthcare concern in the United States. Although the CDC currently lists it as the seventh leading cause of death in the United States, studies show that deaths from diabetes may be underreported. Diabetes may actually be ranked as high as the third leading cause of death in the US. The CDC estimates that more than 100 million adults in the United States are living with diabetes or prediabetes, a condition that if left untreated can develop into diabetes. This number is especially alarming considering that the entire population of the United States was about 325 million in 2017.
Despite these scary statistics, we need to remember that diabetes is a “progressive disease.” This means that it will take a while (potentially years) for Diabetes to reach a point where it can cause other serious health problems. Diabetes is a treatable disease and there are many treatment options. November is National Diabetes Awareness Month, so now is the perfect time to go over some of the basics of diabetes.
What is Type 2 Diabetes?
Although there are a few different types of diabetes, the focus of this article will be on type 2, as 90% of people who have diabetes have Type 2.
Type 2 diabetes is generally known as “adult-onset” diabetes. This is because it becomes more common as age increases, although it is not impossible for children to develop it. In people without diabetes, the pancreas creates a hormone called insulin, which helps the body process and metabolize carbohydrates (sugars) and fats.
In type 1 diabetes, the pancreas is unable to make the insulin. People with type 1 diabetes will always require outside insulin products. In people with type 2 diabetes, however, the pancreas is generally still able to make insulin, but the body does not respond to it. This is called “insulin resistance.” Insulin is an important hormone in the body, and if a deficiency is left untreated, diabetes can develop and cause many other issues in the body. People with type 2 diabetes may or may not need additional insulin depending on a few factors.
Diabetes is generally a preventable disease, but some people are at higher risk than others for developing it. It is recommended that all adults over the age of 45 should be tested every 3 years. Overweight adults with additional risk factors such as low physical activity levels, family history, certain ethnicities, previous gestational diabetes,* high blood pressure, high cholesterol levels, or an elevated hemoglobin A1c* should also regularly get tested. Even if your levels are normal, it is still recommended to screen for diabetes every 3 years. This is important because people with undiagnosed diabetes may not show or have any symptoms until they start having other issues from diabetes.
What Issues Can Diabetes Cause?
Untreated or improperly treated diabetes can result in other issues and complications. Uncontrolled diabetes is associated with heart and cardiovascular complications. People can have their blood sugars fluctuate from low to high if they are not properly treating their diabetes. Other, more serious issues can arise when blood sugar levels are too high for long periods of time, such as eye problems, nerve pain, heart problems, and infections.
Low blood sugar, also called hypoglycemia, happens when blood sugar levels dip below 70 mg/dL. Symptoms of hypoglycemia include shaking, sweating, hunger, racing heartbeat, anxiety or irritability, impaired vision, weakness, headache, dizziness (which can lead to loss of consciousness), seizures, coma, or even death. If you have diabetes, it is important to wear a bracelet, necklace, or another item that identifies you as a diabetic. If you are in need of a diabetes ID item, they can be special ordered at most pharmacies.
It is also extremely important that people with diabetes are able to recognize the symptoms of low blood sugar and know how to avoid it or treat it. Some things that put people at risk for low blood sugar include skipping meals, older age, certain medications for diabetes, alcohol, and sometimes exercise.
Quick Steps to Treat Low Blood Sugar
- Test blood sugar. Low blood sugar is defined as a value that is less than 70 mg/dL.
- If blood sugar is below 70 mg/dL, consume 15 grams of carbohydrates. Some examples include 4 glucose tablets, 5-6 pieces of hard candy, ½ cup of juice or regular soda (not diet!), or 1 tablespoon of honey or sugar.
- These are recommended because the body has quick access to the sugar. Foods like cookies or granola bars are not recommended because the body has to break down the food to have access to the sugar.
- Wait 15 minutes and test blood sugar again. If still below 70, repeat step 2, and then have a meal or snack. If blood sugar is back over 70, have a meal or a snack.
Some other prescription medications can actually hide the signs of low blood sugar. Beta-blockers (metoprolol, atenolol, propranolol, and carvedilol) – medications used primarily for blood pressure control – and are known to mask most of the symptoms of low blood sugar, except for sweating. If you are taking a beta-blocker and have diabetes, it is important to talk to your doctor and make sure that you are closely monitoring your blood sugar, especially if you are prone to low blood sugar episodes.
High Blood Sugar and Diabetes
Alternatively, high blood sugar, also called hyperglycemia, is when blood sugar is over 140 mg/dL or over 180 mg/dL if 2 hours after a meal. Treatment for high blood sugar varies from person to person based on what the doctor has recommended for them and their individual blood sugar goals. Chronic high blood sugar can result in health issues that affect the rest of the body. Complications including eye and vision problems, nerve pain and problems, kidney disease, heart disease, and more can result from hyperglycemia. Depending on age and risk factors, your doctor may prescribe medications for cholesterol (even if you don’t have high cholesterol) and possibly some blood pressure medications.
Peripheral Neuropathy
Around 60-70% of people with diabetes will have some degree of nerve problems and pain due to their diabetes. One of the more common nerve problems is called peripheral neuropathy, which is pain or numbness in the limbs, usually in the legs and feet. This can be a problem as people with peripheral neuropathy often cannot feel their feet as well as someone without it. This makes it easier for infections to happen. Stepping on something sharp, sores from constant rubbing due to shoes that don’t fit properly, and bad skin infections can potentially infect the bone and lead to amputations.
Some signs and symptoms of peripheral neuropathy to be aware of include burning or tingling, the sensation of wearing a sock when one is not on the foot, the sensation of a foreign object in a shoe, or loss of feeling in the area. People with diabetes should inspect their feet every day and become familiar with what is normal for them. Daily checks can help catch any issues or infections before they have a chance to develop into a serious problem. Diabetics should have a foot exam done each time they visit their primary physician. It is also important to make sure to keep feet dry and clean, quickly clean any cuts or abrasions, and properly trim nails.
Managing Diabetes
Managing diabetes can be difficult. It is true that there are a lot of factors that go into making sure you’re staying healthy. Even taking small steps, however, can drastically help improve your health and decrease your risk of complications from diabetes.
The American Diabetes Association has set some guidelines for ideal blood sugar levels at different times of the day. Fasting blood glucose is taken in the morning before breakfast. Post-prandial blood glucose levels are taken 1-2 hours after finishing a meal. Hemoglobin A1c is a percentage that gives a general idea of how well your diabetes has been managed in the past 3 months. Hemoglobin A1c is also a key test in diagnosing diabetes. Suggested levels for each test are in listed on the table below.
| Test Type | ADA Recommended Level |
| Fasting blood glucose (FPG) | 80-130 mg/dL |
| Post-prandial blood glucose (PPG) | Less than 180 mg/dL |
| A1c | Less than 7% |
****It is important to note that these levels are merely guidelines. It is not uncommon for you and your doctor to have set goal values that differ from these.****
Managing Diabetes: The List
There are a lot of things you can do to help you manage your diabetes. To make it a bit easier, I’ve compiled a list of steps you can take to help make managing your diabetes easier:
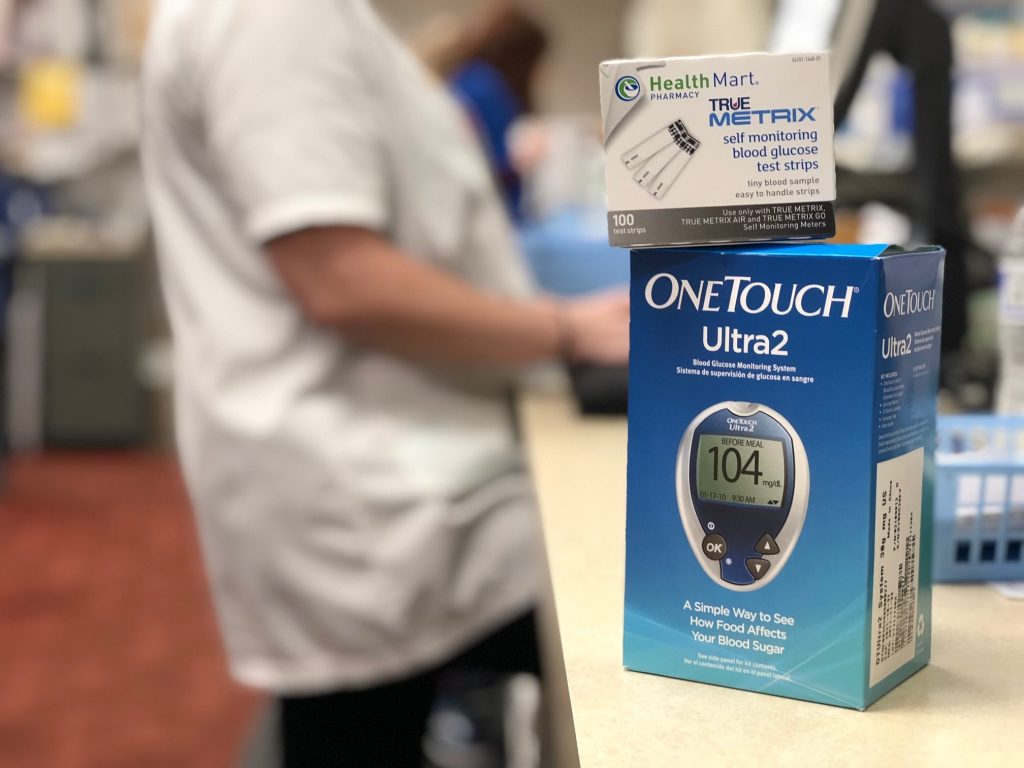
- Speak with your doctor to see how often you should be checking your blood sugar. Know what your personalized goal blood sugars are, and what your action plan is for high or low blood sugar levels.
- Be aware of the symptoms of low blood sugar and what to do if you start feeling the symptoms (detailed above).
- Check your feet daily and become familiar with what is normal and abnormal. Trim your own toenails if you are able. Trim them directly across in a straight line, not curved.
- Keep a list of all of your current medications on you at all times. Wear a bracelet or item that identifies you as having diabetes.
- Develop an exercise plan that is realistic to you and your needs.
- Talk with your doctor or a dietician about changing or adjusting your diet in a realistic way.
- If you have diabetes, make sure you have important vaccinations. People with diabetes should get their yearly flu shot. It is also recommended that you get your pneumonia vaccines. Ask your doctor or pharmacist about which pneumonia vaccine is right for you.
- Keep a log of your blood sugar levels when you measure them. Most blood glucose machines will automatically log them for you, but it is important for you to have an idea of what your trends are without referencing the machine.
Managing Diabetes: The Prescription Tips List
- Make sure you understand how to take all of your medications, including insulin. Rotate insulin injection sites, and keep in mind the abdomen is usually the best area to inject.
- Know the expiration dates for your medications, especially insulin products. Store unopened insulin in the fridge until you begin using it. Below is a general guide for insulin products (always read the vial or prescription label for prescription-specific information).
- Insulin vials are generally good for 28 days at room temperature or in the fridge once they’ve been opened. Levemir vials are the exception and stay good for 42 days once first used.
- Insulin pens are generally good for 10-42 days at room temperature or in the fridge once they’ve been opened depending on the specific type of insulin. Tresiba pens are an exception and stay good for 56 days once used.
- If you are unsure of why you are taking a certain medication, talk to your pharmacist or doctor about it.
- If Insulin shots seem scary, think about this; needles used to inject insulin are smaller than lancets used to test blood sugar!
The American Diabetes Association and CDC websites also have more information and some other good tips.
And don’t forget; your pharmacists here at Oswald’s Pharmacy are here to help if you have any questions!
Definitions:
- Gestational Diabetes: high blood sugar specifically during pregnancy in someone that may not have a previous diagnosis of diabetes
- Hemoglobin A1c: general measurement of a person’s diabetes management over 3 months.